In this three-part blog series, Sr. UX/HF Consultant, Agatha Kalinchenko, MD will discuss the importance of Human Factors from a clinician’s perspective:
The high physician burnout rate together with rising rates of medical errors results in a negative spiral – medical errors can lead to burnout and burnout can lead to medical errors. Please refer to Part 1: Medical Errors are on the Rise and Part 2: Clinician Burnout to learn more about these topics.
The burnout/medical error negative spiral can have a profound negative impact on clinicians. In effect, the patient is not the only victim of medical error. Clinicians have become so negatively affected by medical errors that they have become the “second victims” of medical errors. Clinicians fall victim to often both short and long terms consequences.
THE “SECOND-VICTIMS”
OF MEDICAL ERRORS – CLINICIANS – PART 3

SHORT-TERM EFFECTS
Short-terms effects of making a medical error on clinicians include:
- Fear
- Guilt
- Shame
- Self-doubt
- Anger
- Disappointment
If periods of facing these short-term effects become more frequent or prolonged, clinicians may also face paralyzing long-term consequences.
LONG-TERM EFFECTS
In an article “ The Emotional Impact of Medical Errors on Practicing Physicians in the US and Canada” published in 2007, a survey by 3,171 of the 4,990 eligible physicians in internal medicine, pediatrics, family medicine, and surgery [1] (64% response rate) examined how errors affected five work and life domains. Physicians reported that errors affected the following work and life domains:
- Increased anxiety about future errors (61%)
- Loss of confidence (44%)
- Sleeping difficulties (42%)
- Reduced job satisfaction (42%)
- Harm to their reputation (13%)
- Lower patient satisfaction and care quality
- Higher medical error rates and malpractice risk
- Higher physician and staff turnover
- Physician alcohol and drug abuse and addiction
- Physician suicide
THE IMPORTANCE OF HUMAN FACTORS IN MEDICINE
The large human cost of medical errors on both the patients and clinicians in combination with the growing number of medical errors made creates a critical need for intervention.
As a trained and licensed physician, it seems obvious to me that medical knowledge is not enough to conquer the challenges of a hectic and dynamic healthcare environment to provide consistent and accurate care.
This is where Human Factors (HF) steps in to help support a well-functioning and safe healthcare system. HF focuses on making medical technology safe and effective to use by mitigating potential use errors through a superior user interface (UI) design. A good human factors process not only identifies and mitigates critical potential use errors that can lead to patient harm, but also minimizes usability issues that cause inefficiencies and user frustration.
As an example of a design issued solved by HF, many of you are probably familiar with the problem of tubing mismatches. In this case, a feeding tube was accidentally inserted into a trach tube port and milk was delivered to an infant’s lungs. The result was fatal.[4] However, HF stepped in and was able to help manufacturer’s design solutions by guiding modifications of their devices. These device modifications include the use of bright orange or purple tubing (solid and striped), “enteral-only” labels, and manufacturer-specific enteral-only or non-I.V. compatible connectors.[5]
Indeed, a lot can be done from a UI design standpoint to help lower the high use error rate in the medical world. As a bonus, a good UI design has other benefits beyond increased safety and usability. It can also impact company profitability.
“Research has shown that device design issues including labeling account for 50% of the reasons why there are Class I recalls of 510(k) Device” [6].
As a reminder, Class I recalls are recalls for products which could cause serious injury or death!
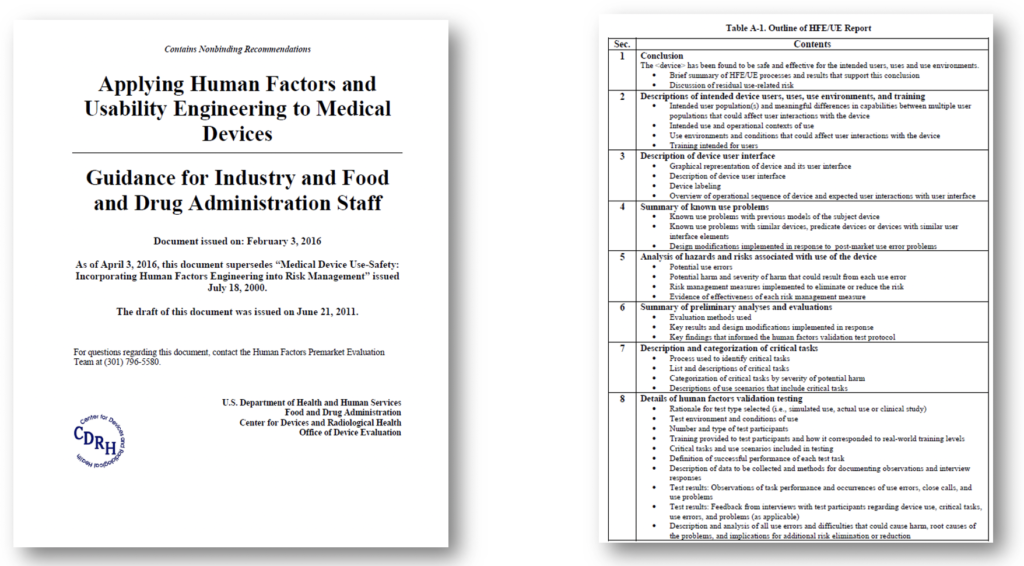
Because the HF process is critical when designing a safe medical product, the FDA has developed guidance documents to assist medical device manufacturers in following appropriate human factors and usability engineering processes. When followed, these guidances maximize the likelihood that new medical devices will be safe and effective for the intended users, uses and use environments [7].
The FDA believes that these guidances will enable manufacturers to assess and reduce risks associated with medical device use and will support manufacturers in improving the design of devices in order to minimize potential use errors and resulting harm!
SUMMARY
GOOD MEDICAL DEVICE DESIGN IS ESSENTIAL
The reduction of medical errors which can be identified and mitigated through the HF process saves not only patient lives, but also improves the lives of healthcare providers in several ways:
- Increased work efficiency
- Improved clinician and patient safety
- Improved quality of care
- Increased time to build strong patient- provider relationships
- Reduced burnout through reduced stress that comes with making medical mistakes
- Improved product success in the marketplace
To help ensure patient safety, clinicians and HF professionals need to join together, forming integrated teams to advance the HF field. We will need as many voices and perspectives as we can to combat the rise of medical errors and the meltdown of our healthcare providers. The emerging result will hopefully meet the levels of safety and effectiveness that we all strive for and have a right to have in our healthcare systems.

BIO
Agatha Kalinchenko, MD – Sr. Human Factors Consultant
Dr. Agatha Kalinchenko is a physician trained at Karolinska Institute in Stockholm, Sweden. Years of clinical exposure to surgery, hospital wards, and out-patient environments helps her bring a physician’s perspective to Sage Research & Design. Her other passion is behavioral science. Agatha earned a Master’s in Psychology from Lund University in Sweden. Her expertise in medicine and interest in the human mind translated easily to the applied fields of user experience and human factors. Before starting with Sage Research + Design, Agatha developed her UX skill set and design knowledge by providing strategic guidance to clients of the digital health company, JOOL Health. Now at Sage, she works as a medical and UX consultant, and is employing proven UX and Human Factors techniques to improve safety and patient satisfaction through improved healthcare product design.
REFERENCES
[1] The emotional impact of medical errors on practicing physicians in the United States and Canada. https://profiles.wustl.edu/en/publications/the-emotional-impact-of-medical-errors-on-practicing-physicians-i
[2] Physician Burnout: Its Origin, Symptoms, and Five Main Causes. https://www.aafp.org/fpm/2015/0900/p42.html#fpm20150900p42-b8
[3] Shanafelt TD, West C, Zhao C, et al. Relationship between increased personal well-being and enhanced empathy among internal medicine residents. J Gen Intern Med. 2005;20(7):559–564.
[4] Examples of Medical Device Misconnections. https://www.fda.gov/medical-devices/medical-device-connectors/examples-medical-device-misconnections
[5] Reduce—and report—enteral feeding tube misconnections. https://journals.lww.com/nursing/FullText/2010/11000/Reduce_and_report_enteral_feeding_tube.22.aspx
[6] Hall, R. Using recall data to assess the 510(k) process. In Public Health Effectiveness of the 510(k) Clearance Process, IOM July 2016.
[7] List of Highest Priority Devices for Human Factors Review. Draft Guidance for Industry and Food and Drug Administration Staff. February 2016. Docket Number: FDA-2015-D-4599 Issued by: Center for Devices and Radiological Health. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/list-highest-priority-devices-human-factors-review

